The healthcare worker shortage plagues healthcare organizations nationwide, paving the way for workforce challenges. From working extended hours to navigating dismal work environments, many healthcare professionals are going on strikes and quitting in droves in response to their work’s mental, physical, and emotional burden.
As the staffing crisis worsens, healthcare leaders are pressed to act promptly and implement a multifaceted approach. By prioritizing this, we can begin to navigate the shortage, ensuring that all patients have access to quality healthcare services.
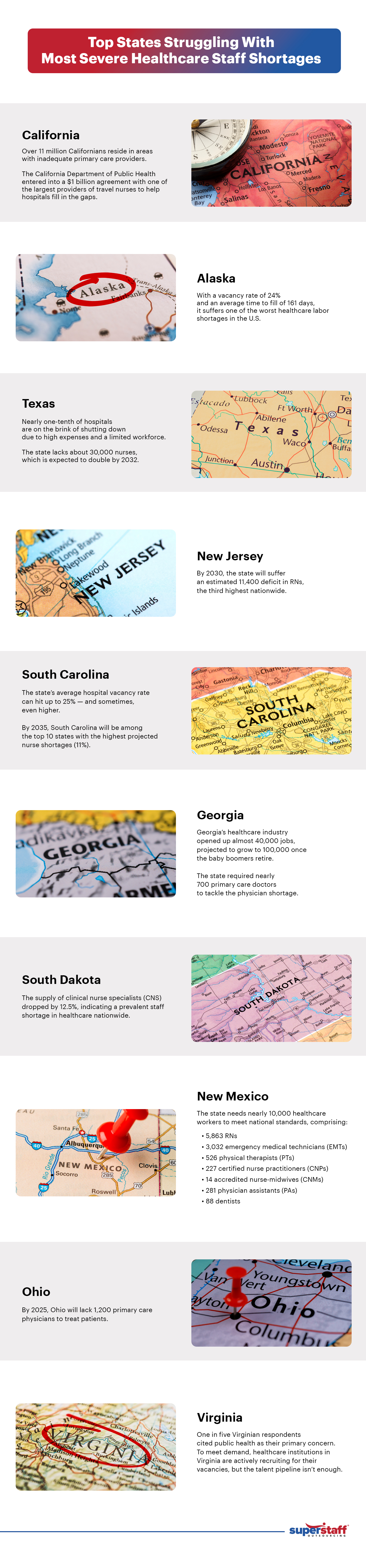
Top States with the Highest Healthcare Staff Shortage
The Association of American Medical Colleges (AAMC) projected a healthcare labor shortage of up to 124,000 medical practitioners by 2034, including 48,000 and 77,100 in primary and non-primary care. Most (91%) of registered nurses (RNs) have cited burnout, poor working conditions, and low salaries as the leading causes of the dwindling number of nurses.
In response to the crisis, the sector is expected to ramp up its recruitment of RNs by 6% from 2022 to 2032.
While the situation is dire across the nation, some states are burdened with more severe shortages — particularly those in rural areas, where access to healthcare is already limited.
So, how bad is the healthcare worker shortage in the country?
California
With its large and diverse population, California has long struggled with a shortage of healthcare workers. The demand for healthcare services in the state is exceptionally high. As such, attracting and retaining qualified professionals has become increasingly challenging.
Over 11 million Californians reside in areas with inadequate primary care providers, causing significant delays in delivering high-quality and appropriate healthcare services. With the worker shortages reaching crisis point, the California Department of Public Health entered into a $1 billion agreement with one of the largest providers of travel nurses to help hospitals fill in the gaps.
Alaska
In 2021, healthcare became Alaska’s top economic sector, opening up about 43,000 annual average jobs and paying nearly $3 billion in direct salaries. But with a vacancy rate of 24% and an average time to fill of 161 days, Alaska still suffers one of the worst healthcare labor shortages in the U.S.
Texas
The second most populous state has far too few healthcare practitioners to meet the healthcare needs of its over 30 million population. However, while the shortage affects the entire state, it is most pronounced in underserved communities where access to essential medical services is even more limited.
Worse, nearly one-tenth of hospitals are on the brink of shutting down due to high expenses and a limited workforce. Currently, the state lacks about 30,000 nurses, which is expected to double by 2032.
New Jersey
The demand for nurses in New Jersey outpaces its supply, with 13,000 nursing jobs remaining unfilled. By 2030, the state will suffer an estimated 11,400 deficit in RNs, the third highest nationwide.
South Carolina
With the lingering impacts of the pandemic, aging population, and low wages fuelling South Carolina’s healthcare workforce crisis, the state’s average hospital vacancy rate can hit up to 25% — and sometimes, even higher. By 2035, South Carolina will be among the top 10 states with the highest projected nurse shortages (11%).
Georgia
The healthcare staff shortages across Georgia existed long before the pandemic. Its healthcare industry opened up almost 40,000 jobs, projected to grow to 100,000 once the baby boomers retire. Recent data also revealed that the state required nearly 700 primary care doctors to tackle the physician shortage.
South Dakota
The state experienced a slight uptick in RNs, from 22,342 in 2022 to 22,684 in 2023. However, the supply of clinical nurse specialists (CNS) dropped by 12.5%, indicating a prevalent staff shortage in healthcare across the state. Moreover, the state’s uneven distribution of nurses contributed to this crisis, as less populated counties have far fewer nurses.
New Mexico
The crippling staffing shortages in New Mexico leave locals no choice but to delay their doctor’s appointments for months, visit out-of-state healthcare providers or occupy hospital emergency rooms for non-urgent medical cases. Research shows that the state needs nearly 10,000 healthcare workers to meet national standards.
Ohio
The labor shortages in Ohio’s healthcare system have been detrimental, especially to locals needing medical assistance. Unfortunately, the problem is bound to get worse. By 2025, Ohio will lack 1,200 primary care physicians to treat patients. As such, the legislation proposed a bipartisan bill to combat Ohio’s nursing shortage and guarantee quality patient care, starting during the pandemic.
Virginia
One in five Virginian respondents cited public health as their primary concern. To meet demand, healthcare institutions in Virginia are actively recruiting for their vacancies, but this may not be enough.
The state’s rural nature also contributes to difficulties in recruiting healthcare professionals. As a result, residents, particularly those in remote areas, face significant barriers to accessing necessary medical care.
Factors Driving Healthcare Staffing Shortages
The healthcare worker shortage (2023) in the U.S. isn’t just a mere inconvenience but a public health concern causing increased hospital-acquired morbidities, patient falls, and even the possibility of death.
But why is there a healthcare worker shortage in the first place? Let’s see:
Aging Population
The rapid aging of the U.S. population is slowly becoming a “national emergency.”
To compare, the under-18 population expects a growth projection of only 5.6%, but the aging population (65 and older) will soar 42.4% by 2034. This has increased the demand for physicians from 280,700 in 2019 to 407,300.
The rise of the aging population also drives swaths of healthcare practitioners out of the field as more baby boomers reach retirement age — with over two-fifths of active physicians being 65 or older in the next decade.
Limited Talent Pipeline
An overwhelming 74% of recruiting managers agree that the skills gap persists across several sectors — and the healthcare industry is no exception. Only a limited number of people are entering the healthcare workforce, contributing to the shortage of doctors, nurses, and even home health aides.
With the expected surge in the population suffering from chronic illnesses, employers seek healthcare professionals with the necessary know-how and soft skills to ensure quality care, connect with patients, and de-escalate tense situations.
However, the emergence of automated and digital communications restricts face-to-face interactions, causing healthcare services to be less patient-centric. Worse, emojis and casual acronyms are now pervading professional communications, which can taint the credibility of formal documentation and the ability to exchange information.
Burnout
The realities of the healthcare industry are taking a toll on the well-being of its personnel, leading to burnout.
Even before the pandemic, physicians already faced twice the risk of burnout compared to the general population — what’s more, 40% of healthcare workers also experienced depression and suicidal ideation. The situation worsened during the pandemic, with up to 75% of clinicians suffering signs of burnout, depression, sleep disorders, and trauma.
As a result, about 20% of the healthcare professionals left during the period — and 80% of those who stayed reported how the labor scarcity affected their work performance. Research further showed that nearly all healthcare workers worry that their burnout will reduce the quality of patient care.
Insufficient Training Programs
The impact of staff shortage in healthcare has trickled down to medical schools, causing enrollment restrictions due to a lack of nursing facilities, clinical sites, classroom spaces, and budget constraints amid the growing demand for healthcare professionals.
A study found that U.S. nursing schools turned down 91,938 qualified applicants from degree and graduate programs, citing a “shortage of educators” as a primary reason for their rejection.
Meanwhile, 909 nursing academies nationwide survey identified 2,166 full-time faculty vacancies. On the other hand, schools with no vacancies were reported to need an additional 128 faculties to fulfill student demands.
Pandemic-Related Pressures
The COVID-19 pandemic has put additional stress on the healthcare system, amplifying the shortage of healthcare workers.
Several healthcare institutions temporarily shut down during the first two months of the pandemic to inhibit the outbreak, losing about 1.5 million healthcare jobs. During the succeeding Omicron surge, the healthcare sector also grappled with critical staffing shortages, which peaked at 22% during the second week of January 2022.
Since then, many displaced employees have returned to work. Yet, the labor participation rate in healthcare remains underwhelming, with the workforce dropping by 1.1%, or 176,000, compared to February 2020.
Strategies for Addressing the Shortage
Since the healthcare worker shortage is a complex, long-standing issue stemming from different factors, solving it requires an equally multifaceted and long-term approach.
As such, we’ve laid out a comprehensive guide for potential solutions to the shortage.
Invest in Healthcare Education
Hospitals and clinics across the U.S. desperately need new generations of healthcare professionals. They can establish their own education entities or partner with accredited educational institutions to address this pressing challenge.
For instance, a healthcare entity can design proprietary and highly customized programs and curriculums to tackle specific healthcare needs and develop industry skills. From a hiring perspective, this can be an effective solution to draw in entry-level professionals, enabling them to advance in their careers. In doing so, employers will only need to focus on upskilling high-demand jobs instead of seeking candidates who may or may not align with the job description.
Furthermore, healthcare entities can provide educational grants to students pursuing medical school to reduce turnover rates. A study showed that 80% of program candidates receiving these benefits remained with the company until the end of the year — a steep jump compared to only 56% for those without benefits.
Strengthen Existing Workforce to Optimize Retention
The simplest yet most often overlooked employee attraction and retention strategy lies in focusing on your existing employees. You can onboard as many hires as possible, but it won’t stabilize your workforce if you’re still hemorrhaging your core staff.
One of the most crucial aspects of building your workforce is to tend to the needs of your employees. Here, you can balance extrinsic and intrinsic rewards. While lucrative pay and benefits are imperative for retention, their psychological well-being is equally important.
All healthcare workers need to feel valued in their organizations. As their employers, you must acknowledge and accommodate their cultural, generational, and gender diversity. Our staff will be likelier to stick around if they’re empowered and listened to instead of searching for greener pastures.
Implement Flexible State Licensing Requirements
During COVID-19, several states eased licensing requirements to allow internationally trained healthcare workers to fill critical roles. Beyond the pandemic, more states should follow suit and implement similar policies to address the ongoing healthcare worker crisis.
Recruiting from states that are not as severely affected by the shortage can also pave the way toward the equal redistribution of healthcare workers nationwide.
Currently, the U.S. is home to 270,000 trained healthcare professionals who are either underemployed or unemployed.
Address Burnout and Attrition
Most healthcare jobs are unsustainable because of their inherent nature — fast-paced, high-pressure, and exhausting. Because of this, most medical staff end up overworked, putting them at risk of burnout.
In a recent poll grading organizations’ efforts in addressing burnout, clinicians rated themselves a “C–.” They identified several unnecessary and mundane tasks that consumed their time from delivering quality patient care, such as:
- Assignments that fulfill administrative requirements (32%)
- Work that could be performed by others or through automation (20%)
Healthcare workers already have enough on their plates. To offload their burden, clinics and hospitals must optimize workflow by leveraging technology and automation. This, in turn, can improve staff productivity and drive down burnout.
HCA Healthcare, a leading healthcare provider, has already initiated this effort. For one, the company is experimenting with a generative AI solution that extracts relevant data from physician-patient interactions to organize and create medical notes — ultimately offloading the task from overburdened healthcare workers.
Specialty Healthcare Outsourcing
Another great strategy to combat burnout among healthcare professionals is delegating repetitive, non-clinical, low-value tasks to a healthcare BPO. Integrating outsourcing solutions allows medical institutions to speed up task completion, minimize costs, and optimize business processes.
Especially with the soaring demand for healthcare services, hospitals and clinics will require professional help to manage their patients, workforce, and operations.
Some non-core tasks you can outsource include:
- Medical Transcription: Transcribing audio recordings from physicians and other healthcare professionals into written documents
- Medical Billing and Coding: Translating injuries, diagnosis, and medical procedures into alphanumeric or numeric codes. Medical billers receive the information and submit claims to the insurance company.
- Healthcare Virtual Assistant Services: Managing patient requests and concerns, scheduling appointments, and updating patient records when necessary
- Medical Call Center Services: Handling complaints, feedback, or grievances on their patient experience
- Insurance Claims Processing: Validating the insurance claims and preparing claim payments
- DME Billing & Collections Ticket Reviewers: Submitting and reviewing claims on durable medical equipment (DME)
Navigate the Healthcare Worker Shortage With SuperStaff
There’s no denying that immense perseverance and top-notch strategies are the best tools to combat healthcare staff shortages. Coupled with innovative ideas, modern approaches, and a dedication to positive changes, healthcare organizations can sail through the storm smoothly.
SuperStaff, a trustworthy BPO provider, can address your unique workforce challenges and simplify recruitment processes. Amid the dwindling number of healthcare professionals, we’ll deliver only the best solutions to catapult your healthcare organizations to new heights.